As the technology infrastructure in hospitals matures, digital health leaders look to integration.
With systems sharing data across platforms and with personnel, we expect significant strides forward in patient outcomes and hospital efficiency.
This is the next in our series checking up on digital health topics in 2025.
“At its simplest, interoperability is the ability to move information easily between people, organisations, and systems. It enables a connected healthcare system that shares health information securely, safely and without any special effort from the people and organisations involved.
… Connected care benefits healthcare providers by providing them with timely access to the permitted information they need, in a format that allows them to effectively improve clinical decision-making and care.”
Australian Digital Health Agency (ADHA) in the National Healthcare Interoperability Plan (PDF).
There are many visions of interoperability.
The Australian healthcare system has many layers. Even within a specific topic such as ‘interoperability’ there are different areas of focus. One key example is ADHA’s objectives to have patient data sharing between primary (your GP) and acute (hospital) care, as well as out-of-hospital specialists, allied health, and long-term care such as residential facilities.
Ikonix Technology’s expertise is in delivering critical messaging systems. In doing so there are elements that associate with these system-wide initiatives as we convey data from source to destination. Importantly we also connect the technologies that run the hospital itself, often excluded from the broad examinations of interoperability. Integrating systems inside a hospital brings in the security, facility management, clinical and communication systems that keep acute care operational. It is from that perspective that we examine interoperability.
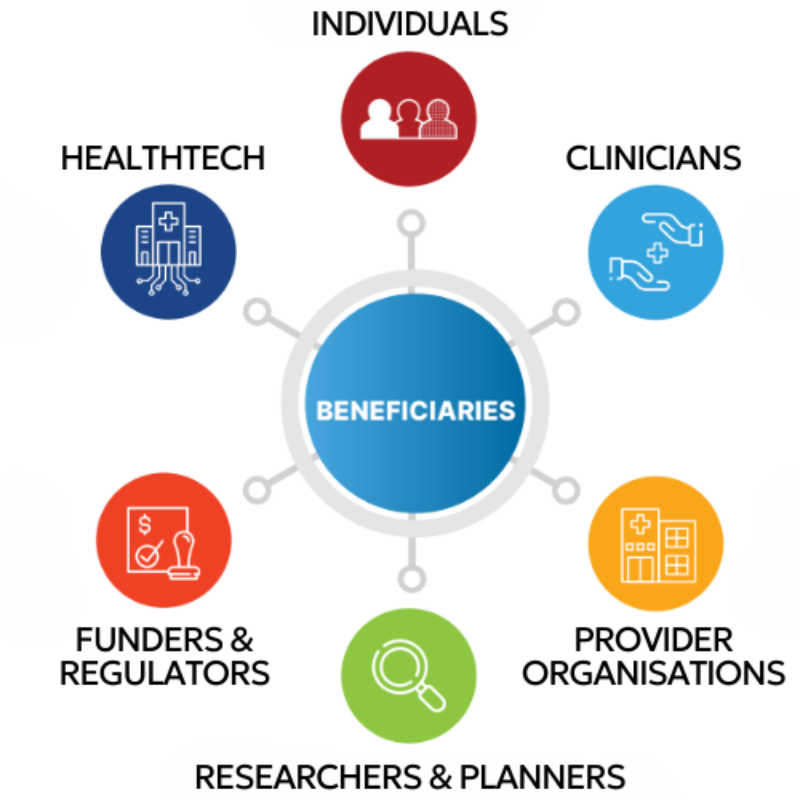
Image: ADHA’s benefits of interoperability connect the technology sector (including Ikonix Technology), as well as our customers, their personnel, and the clients. Graphic adapted from ‘Connecting Australian Healthcare’
What is the current state of interoperability?
Information transferring between systems.
One of the Principles of the ADHA’s National Healthcare Interoperability Plan (NHIP) is for the ‘capture, sharing and managing’ of clinical data to be a major aspect of investments in digital health.
This often delivered by disparate measurement and monitoring systems, and archival and reporting via an Electronic Medical Record (EMR). Most Australian states have or are implementing a system-wide EMR for their health authorities. Difficulty arises for integrating systems when selected vendors differ between jurisdictions.
This conflict may be resolved by the implementation of data standards, such as HL7 or FHIR. These structure information so that it can be shared more easily, using a common language across vendors and technologies.

Timely access to information.
Under the ‘Innovation’ priority area of the NHIP, the Agency discusses the ‘clinical insights’ delivered by the ‘near-real-time sharing of data’.
Though system integration and automation, software shares the data to make it accessible to clinicians almost immediately. Without the need to chase down diagnostic reports or other media, or collate several sources themselves, a doctor can make an informed treatment plan in less time, with obvious patient wellbeing outcomes.
We can extrapolate and suggest that faster decisions would also improve patient flow through the hospital, boosting efficiency and bed turnover rates.

Improving clinical decision-making.
A further Principle of the NHIP is the need for data integrity, with information validated against ‘sources of truth’. This follows investment in the collection and governance of information and necessarily leads to the quality of clinical decision-making that can be achieved. The Principles also outline that data should be entered in a single place, and then used across multiple platforms, to alleviate the inefficiency of manually cross-pollinating information.
By creating networks of interoperable services in our healthcare system, clinicians enter their data once and have access to well-populated information about their patient, to make the best decision for their wellbeing.

Why do our customers expand their communication interoperability?
Ikonix Technology brings together clinical systems, building infrastructure, and communication networks. This helps ensure clinicians and hospital operators have the information they need to make life saving decisions quickly, easily, and reliably, or keep a complex facility running.
Connected systems sharing data for long term archival or triggering next steps.
Automation to support hospital workflows and reduce burden on personnel.
The speedy transfer of data facilitates faster, more reliable decision-making.
Vital data is served to an endpoint where clinicians need, so they can focus on the patient.
Integrated systems.
By integrating technologies and the communication stack, Ikonix Technology brings together human and digital sources of information, allowing clinicians to focus on the patient.
Such integrations are built using existing interoperability communication standards such as FHIR and HL7, application- or industry-specific options, or are fully custom and developed for that solution alone.
Thought Ikonix Messenger we already integrate more than 90 different systems:
- Clinical solutions such as nurse call systems,
- Operations and facility systems such as the hospital’s Building Management System (BMS), and then
- Communication outputs, from the PABX and SMS to encrypted paging.

Automation.
To alleviate burden and smooth the process between systems, Ikonix Technology works with out clients to deliver automated actions. These are customised to meet the unique needs and existing methods of the customer. Examples include
- An RTLS event, such as a duress tag being pulled, dispatching that information out to multiple security teams, including self-selecting the recipient by location,
- Pre-configured on-call rosters updating call traffic flows, to direct contact requests to the on-shift personnel, or
- Patient discharge systems generating a bed cleaning task.
By developing an order in which systems trigger one another and personnel involvement we reduce the touchpoints and effort demanded of the hospital workforce.

Timely data.
Choosing the medium for delivery is a key decision in providing time-sensitive information-sharing. For example,
- Paging messages use a local, private and resilient radio network. In hospitals using Ikonix Encode, such as the HIRPN network across Sydney, receive priority alerts in just three seconds,
- SMS is a ubiquitous messaging system and can be deployed either via an on-site modem or through a third-party gateway, but can take as much as 30 seconds or more from dispatch to receipt, and
- Communication apps like those within productivity suites or available at a consumer level see their data travel through international servers and prompt a basic tone or vibration for the receiver. Critical messaging-specific apps such as Ikonix Connect can break through a phone being on silent ensuring propriety messages achieve a quick response.
Messages for non-critical situations such as organising lunch could utilise one medium, while a Code Blue would likely require another.

Supporting clinical data.
Beyond the integration of systems using a messaging specification such as FHIR, clinical messaging solutions need to take steps to further support the hospital environment. Where consumer apps might provide many of the features a clinician might utilise, they don’t or can’t incorporate important customisations.
In our experience supporting clinical messaging and developing Ikonix Connect, we’ve identified several important use cases:
- Secure media sharing. Where other systems would store photos or videos on an unknown cloud server, it’s vital for patient privacy that rich media is kept secure.
- Role-based messaging. With a workforce in the thousands, clinicians often won’t know the specific person they need to access for consultation, and so helping them contact the Role ensures the right support,
- Critical and integrated alerts. Many consumer or generic communication platforms simply cannot integrate many if any other solutions, forcing hospital personnel to use multiple and disparate systems, creating inefficiency. These also usually cannot send information with any greater degree of urgency, such as the breakthrough alerts discussed above.


