The wellbeing of Australia's junior clinicians is paramount for the health system.
As burnout and communication breakdowns impact Australia’s junior doctors, nurses and frontline clinicians, Ikonix Connect offers a possible solution.
In Australian hospitals, junior doctors, nurses, and other frontline clinicians are under mounting pressure. Long hours, frequent handovers, and inefficient communication channels contribute to widespread burnout and dissatisfaction.
The recent AMA Western Australia Hospital Health Check report revealed that while some working conditions have improved for junior doctors, many still face excessive workloads and lack systemic support.
The report surveyed hundreds of junior doctors, with the largest cohort of responses from adult medicine (physician) (22.6%), surgery (13.3%), emergency medicine (12.4%) and paediatrics (8.7%).

The AMA-WA’s report card gave wellbeing and burnout grades of C and D to all but one organisation (St John of God received a B).
As much as 41% of responding junior doctors report spending two to four hours on admin tasks during an average shift and notably explain that they see “little point in trying to get help from IT or other resources.”
In this ongoing publication, the AMA-WA identified that the reviewed category of terms, rosters and workloads has seen the most significant decline in results to 2025, compared with prior years, suggesting that these conditions are getting worse for junior doctors. Only one employer improved, and that was to a C-grade, up from a D in 2024.
The junior clinician experience, as quoted in HealthServicesDaily:
“Weekend on calls for some specialties are just mad. I received over 150 calls a few weekends back. Non-stop. … To be honest, it’s not a safe working environment for patients or staff”
“Being awake and giving phone advice all night for $12 an hour and being expected to work all of the next day is not appropriate.”

This survey’s results align with the similarly titled publication from the AMA in South Australia. In SA the data comes from a different source, the 2024 Medical Training Survey. This Survey is conducted yearly by independent researchers, and endorsed by the AMA and regulators.
The 2024 (most recent) report highlights the proportion of junior clinicians working more than 50 hours per week, across Adelaide hospitals. These are relatively static from 2023, though with a notable improvement at the Royal Adelaide Hospital.
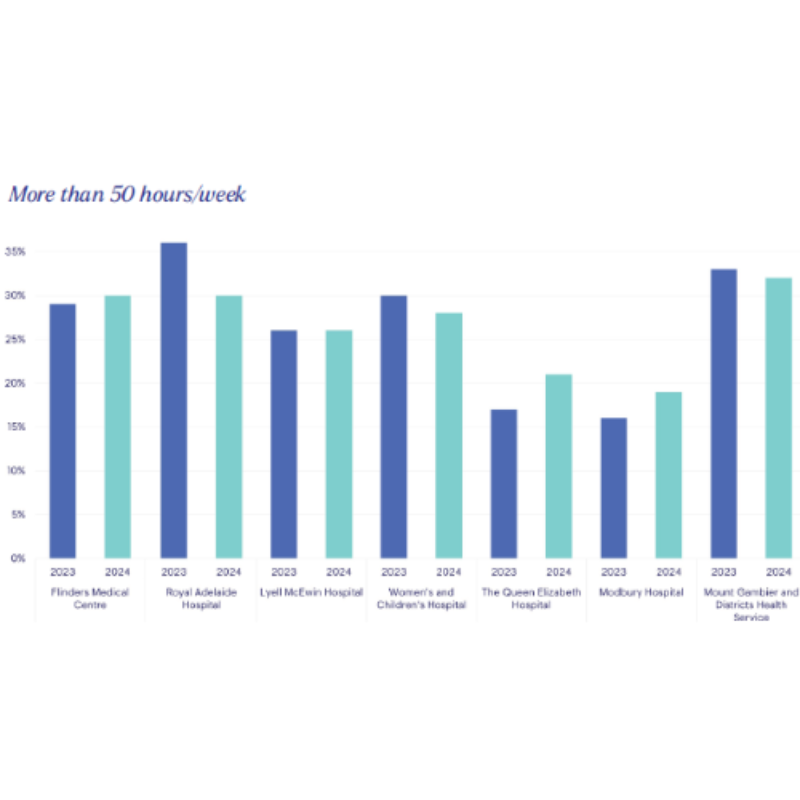
At a national level, looking at the Medical Training Survey, 62% of junior doctors are working more than 40 hours a week, with 9% completing, on average, more than 60 hours.
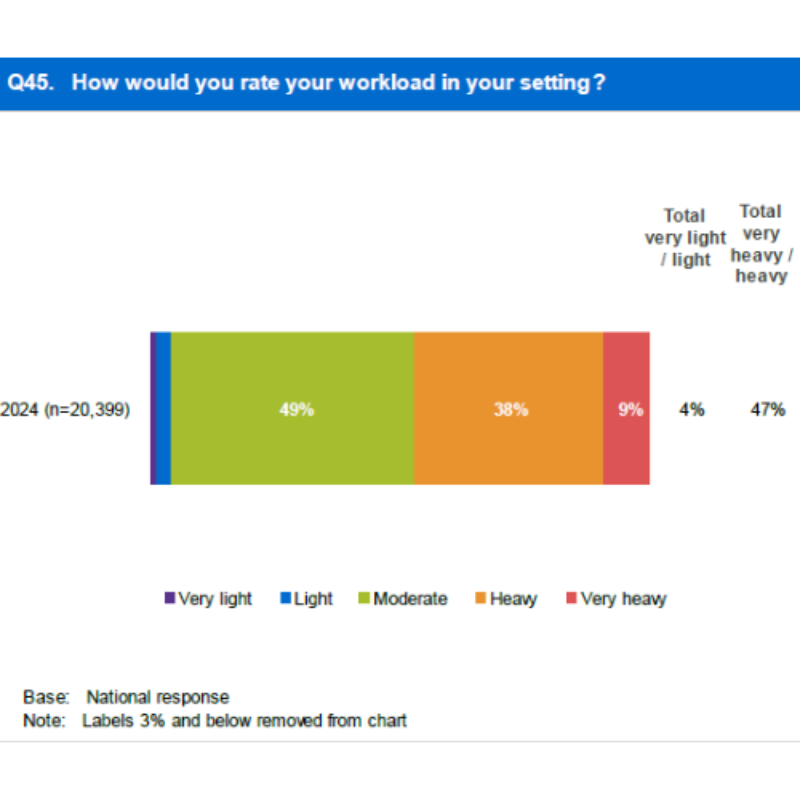
Almost half (47%) self-rated their workload as ‘heavy’ or ‘very heavy.’ One in five (21%) report working unplanned overtime ‘always’ or ‘most of the time’ with negative impact on their training.
25% of trainee doctors confirmed work volumes impacted their wellbeing, and 18% report negative wellbeing effects from working unpaid overtime.
Burnout is not isolated to doctors. Nurses and allied health workers face parallel struggles—managing competing priorities, responding to unclear or delayed communications, and frequently being contacted after hours.
The root cause often lies in fragmented systems and a lack of streamlined collaboration tools. When communication is slowed or misrouted, the result is a rise in avoidable errors, delayed decisions, and increased stress across entire care teams.

How can Ikonix Connect support clinicians to avoid burnout?
Ikonix Connect can contribute to managing workload in two keys ways:
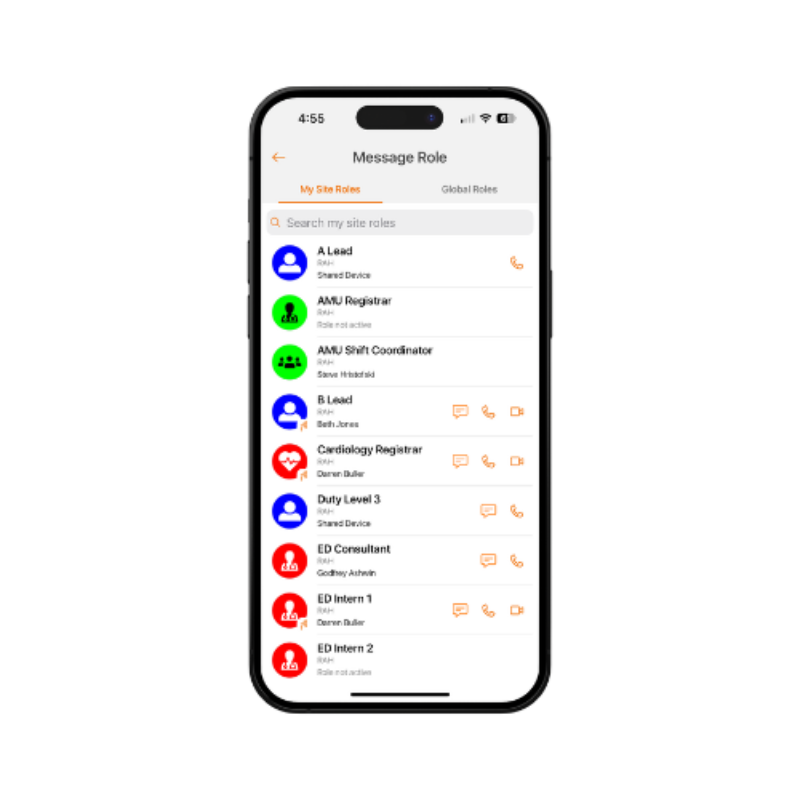
Firstly, whether it's a doctor finishing a night shift or a nurse handing over to the next team, continuity and accountability are crucial. Ikonix Connect’s role-based messaging and on-call rostering handovers help ensure safe transfer of responsibility.
Unlike consumer messaging apps, Ikonix Connect lets clinicians pass roles within a team to ensure unbroken coverage and automatically directing other personnel to the correct on-call clinician. This means fewer out-of-hours contacts, and certainty for the rest of the hospital that someone is online and ready to consult.
With the introduction of Australia's “Right to Disconnect” legislation in 2024, it became imperative to support clinicians' ability to disconnect from work communication during personal time.
Ikonix Connect allows all staff to set availability statuses. When a clinician toggles offline, communications directly to them are delivered silently and stored for when they return, preventing unnecessary disruption and supporting a culture of respect and work-life balance. Colleagues can easily see the user’s online status, and when contacting a Role for the online on-call person, communication is routed to someone available to help, allowing the proper break for the offline clinician.

The wellbeing of our healthcare professionals—doctors, nurses, and all frontline staff—is vital to the functioning of Australia’s health system. Ikonix Connect addresses some of the most pressing causes of burnout by streamlining communication, protecting personal time, and fostering efficient, accountable team collaboration. By embracing tools like this, hospitals can create safer, more sustainable working environments for all clinicians, ensuring better outcomes for both staff and patients.


